Sesamoiditis
Sesamoiditis is a condition in which the sesamoid bones in the forefoot become inflamed from physical activity. Sesamoid bones are bones that are not connected to other bones but are located in tendons or muscle. Two of these sesamoid bones are very small and located on the underside of the foot near the big toe. Athletes such as runners, baseball and football players, and dancers are likely to experience sesamoiditis. Those with high arched feet, flat feet, or runners who run on the ball of their foot are also prone to suffer from sesamoiditis.
Symptoms include pain or throbbing on the ball of the foot near the big toe. The pain generally starts with a mild throbbing but gradually builds up to shooting pain. Bruising, swelling, and redness are possible, but in most cases, these symptoms are not present. However, moving the big toe can result in pain and difficulty.
To conduct a diagnosis, the podiatrist will examine the ball of the foot and big toe. They will look for any outliers and check the movement of the toe. X-rays will be taken to rule out any other conditions and ensure that it is sesamoiditis.
Treatment for sesamoiditis is generally mild and includes rest, anti-inflammatory and pain medication, and ice treatments to deal with the swelling and pain. Orthotics may be needed with people who have flat or high arched feet to relieve pressure off the bones. In some cases the toe will be taped and immobilized to allow healing. The podiatrist may also decide to use a steroid injection to help with swelling as well. If you have sesamoiditis, you shouldn’t engage in any intensive activity, as it may inflame the area and worsen your pain. If the sesamoid bone has fractured, surgery may be required to remove the sesamoid bone.
If you are suffering from sesamoiditis or are experiencing symptoms similar to sesamoiditis, you should stop all physical activity that puts strain on the area. Furthermore you should see a podiatrist for a diagnosis to see if you have sesamoiditis.
Causes and Diagnosis of Athlete's Foot

Athlete's foot, medically known as tinea pedis, is a fungal infection that affects the skin on the feet. It is causes itching, burning, and cracked, scaly skin, often occurring between the toes. The infection is caused by dermatophytes, fungi that thrive in warm, moist environments such as locker rooms, showers, and swimming pools. Athlete's foot spreads through direct contact with an infected person or by touching contaminated surfaces. Diagnosis typically involves a physical examination of the affected area by a podiatrist. In some cases, a skin scraping may be taken and examined under a microscope to confirm the presence of the fungus. Proper diagnosis is important to differentiate athlete's foot from other skin conditions. If you have any of the above symptoms, it is suggested that you consult a podiatrist who can effectively treat athlete’s foot, which may include prescribed medication.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Ramin Nadjafi, DPM from Advanced Podiatry Group. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Orlando, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete’s Foot
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into the cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder in shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.
Types of Ankle Surgery for Arthritis

Ankle arthritis, marked by the deterioration of the cartilage in the ankle joint, can cause significant pain and hinder movement. When conservative treatments like braces, cortisone injections, and physical therapy fail to alleviate symptoms, ankle surgery may become necessary. For mild to moderate arthritis, minimally invasive surgeries can help by cleaning out inflamed tissue and removing bone spurs to restore range of motion and reduce pain. In more severe cases, ankle fusion or ankle replacement might be required. Fusing the bones of the ankle can help to eliminate pain, though it reduces flexibility. In contrast, replacement of the damaged joint with an artificial one offers better movement but with a longer recovery period. Cartilage repair techniques can help regenerate damaged cartilage. Another option involves using an external device to stretch the joint, which allows space for cartilage repair. Each surgical method has its benefits and considerations, making it essential to discuss with a podiatrist which option is best suited to your condition. If ankle arthritis is impacting your life, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with Ramin Nadjafi, DPM from Advanced Podiatry Group. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our office located in Orlando, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Pain
Pain experienced in the ankle can be caused by a multitude of conditions. While the most common cause is an ankle sprain, other possible problems can include arthritis, gout, ankle instability, an ankle fracture, nerve compression, or tendinitis. In more serious cases, ankle pain can be a sign of improper alignment of the foot or an infection.
Ankle pain can often be accompanied by symptoms such as redness, swelling, stiffness, and warmth in the affected area. Pain can be described differently depending on the condition: short, stabbing pain and a dull ache are some examples. If such symptoms are persistent and do not improve after time, be sure to schedule an appointment with your local podiatrist.
Depending on the condition causing your ankle pain, different treatments may be prescribed by your podiatrist. For ankle sprains, the first step in treatment involves rest, ice, elevation, and compression. Be sure to avoid placing pressure on the ankle, use an ice pack several times a day, and use a compression bandage and elevation to reduce swelling. Other, more serious conditions may require the assistance of certain drugs and medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, or even cortisone injections.
Depending on the severity of your ankle pain and the condition behind it, recovery from ankle pain may take some time.
Consult with your foot and ankle doctor to best determine the cause of your ankle pain and the appropriate treatment.
What Are the Causes and Symptoms of Toenail Fungus?
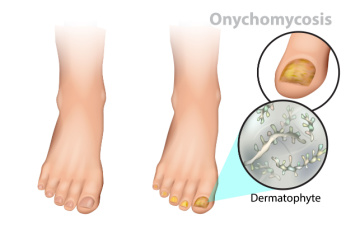
Toenail fungus, or onychomycosis, is a common infection that affects the toenails, caused by various types of fungi. It often starts as a white or yellow spot under the tip of the toenail and can spread deeper, leading to discoloration, thickening, and crumbling at the edges of the nail. Causes of toenail fungus include exposure to damp environments, such as public showers or pools, wearing tight shoes, and having a history of athlete's foot. Symptoms include nails becoming discolored, brittle, and misshapen, sometimes accompanied by a foul odor. The affected toenail may also separate from the nail bed, causing discomfort. Proper foot hygiene, keeping feet dry, and avoiding shared nail care tools are preventive measures. Early treatment is important to prevent the infection from spreading and to restore nail health. Toenail fungus can be unsightly and can affect the skin on the feet. If you have developed this infection, it is suggested that you visit a podiatrist who can effectively treat toenail fungus.
For more information about treatment, contact Ramin Nadjafi, DPM of Advanced Podiatry Group. Our doctor can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our office located in Orlando, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
Location of Foot Pain May Indicate the Cause

Foot pain can affect various areas of the foot, each indicating different underlying causes and requiring specific treatment approaches. Pain in the heel, for example, may signal conditions like plantar fasciitis, Achilles tendonitis, or heel spurs, often treated with rest, stretching exercises, or orthotic inserts. Pain in the arch of the foot may result from conditions such as flat feet, plantar fasciitis, or overuse injuries, requiring supportive footwear, arch supports, or custom orthotics for relief. Pain in the ball of the foot could be due to metatarsalgia, Morton's neuroma, or sesamoiditis, necessitating cushioned insoles, proper footwear, or corticosteroid injections. Furthermore, pain in the toes may indicate issues like bunions, hammertoes, or ingrown toenails, often managed with padding, splinting, or surgical intervention. By pinpointing the location of foot pain and understanding its potential causes, a podiatrist can offer appropriate treatment methods to alleviate discomfort and promote foot health. If you have foot pain or discomfort, it is suggested that you make an appointment with a podiatrist for an accurate diagnosis and the appropriate treatment solutions.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Ramin Nadjafi, DPM from Advanced Podiatry Group. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Orlando, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.